2005-2010/Part 4: My phenomenal immune restoration and beyond

2005: ‘Maureen the Switch Bitch’ aka ‘The Pox Doctor’s Clerk’
By the time January 2005 rolled around, I had been at the Holden Street Sexual Health Clinic (HSC) in Gosford for a year and had well and truly settled into my substantive position as the clinic’s sole Administration Officer. HSC wasn’t the first health care setting that I had been employed at, however it was the first time I had held a non-commercial/military logistics and inventory control position in health care.
My first health workplace setting was in 1982–1985 when I was the Petty Officer in charge of the Hospital Medical Store at HMAS Penguin in Balmoral, Sydney. The second was in 1996–1997 when I was employed as the Inventory Control Officer (Operating Suites) at the Mater Misericordiae Hospital in North Sydney. I thoroughly enjoyed working at all these health settings, however HSC provided the most dynamic and rewarding experience where I interacted and supported a small multi-disciplinary team of clinicians while also supporting not only clients with general sexual health issues, but also people living with HIV/AIDS.
My primary role amongst many other administration functions was staffing the front-of-house reception and I often referred to myself as ‘Maureen the Switch Bitch’. I was trained to triage clients to learn whether they were part of our priority population groups and then making appointments as required. The official address for HSC is 69-71 Holden Street Gosford, however it was standard practise to drop the ’71’. Without a doubt, new clients found it very amusing when told the clinic was located at 69 Holden Street, the irony was not lost on them. Not long after starting there I found myself needing to seek more specific HIV health information for my own needs from staff who I had come to appreciate and admire and who accepted me as part of the small team. I was still travelling to Newcastle for my HIV monitoring, usually on my acquired days off (ADOs). The Clinic Director; Dr Debbie Allen and the Career Medical Officer (CMO) in HIV/Sexual Health, Dr Kym Collins were always keen to hear about my ongoing topsy-turvey HIV antiretroviral struggle, drug resistance and adverse reactions.
In 2005, I continued studying online with Sydney University for my Graduate Diploma of Health Science (Sexual Health), which I had started in late 2003 when it was a face-face course known as the Diploma of Sexual Health Counselling and administered through the Australasian College of Sexual Health Physicians and Sydney Sexual Health Centre at Sydney Hospital. I also began studies with NSW Health for the Certificate 3 in Business in April 2005, so study wise I was kept very busy in my spare time.
2005: Training another Positive Speaker Service
The local Central Coast HIV care and support service, Positive Support Network (PSN) wrote to me in June 2000 when I was co-ordinating the Positive Speakers Bureau (PSB) expressing an interest in having a training proposal put together for myself to visit Gosford to conduct training, so that it could have its own local people doing positive speaking engagements. A proposal was put together and sadly at the time did not go ahead due to the lack of funding by the PSN. Knowing my previous background in positive speaking co-ordination, in early 2005 I was asked by the then Central Coast Area Health Service (CCAHS) HIV and Related Programs (HARP) Manager, Karen Nairn whether I would consider conducting training for members of the PSN. Ironically the area health service had found funds to support the training for the PSN. So, after planning and recruiting for suitable trainees, I agreed to do two weekend workshops which resulted in the PSN having its own Positive Speaker Service (PSS) with six new positive speakers. Little did I know at the time that I would take over as the manager of the PSN five years later, and that PSS would go on to prosper in a similar way to that of its city cousin, the Positive Life PSB.
2005: Chronic Disease Self-Management
In July 2005 I was selected to undertake training for the CCAHS Chronic Disease Self-Management Program (CDSMP) which was based on the Stanford University model in the USA. I became one of the project’s workshop leaders and so began a ten-year association with that Program doing seven workshops (one a year) at local Neighbourhood Centres which would each run over six weekends. During this time, I also initiated, planned and facilitated three specialised CDSMP workshops for HIV/Sexual Health, PSN and women living with Hepatitis C/HIV. It was extremely rewarding seeing people not coping very well, sharing their lived experiences and gaining new skills in a non-threatening and supported environment often empowering them to better cope with their chronic illness.
I successfully gained both my Grad Dip of Health Science degree and Certificate 3 in Business in March and April 2006 respectively. I thought I was done with studying however, eight years later I found myself studying Training, Assessment and Evaluation (TAE) in preparation for applying for Community Services part time casual teaching position for the Hunter Institute of TAFE (now TAFE NSW).
2006: Dangerous Hypersensitivity and another Opportunistic infection
Twenty-six months at HSC had come and gone very quickly and my employee/patient status at the clinic suddenly changed. I needed an urgent in-house consultation with the Dr Kym Collins, due to experiencing ongoing unexplained worsening chronic diarrhoea and weight loss over the previous four months. Stool cultures which Kym ordered failed to show any growth, ova cysts or parasites, microsporidia, cryptosporidium nor giardia antigens. Kym referred me to a local gastroenterologist Dr John Dowsett, who after reviewing me in early May scheduled an endoscopy/colonoscopy four weeks later at Gosford Hospital. I have a family history of anal and colon cancer (my father, but he did not die from either) and coupled with my earlier history of opportunistic infection with Kaposi’s Sarcoma (KS) in 1998, John was concerned that I might have had internal KS or Mycobacterium Avium Complex (MAC) or other significant infection/neoplasm.
Two weeks (13 May 2006) before the procedures were to take place, I fronted at work as usual. This time, I was covered from head to toe with tiny red blotches which had developed overnight. Dr Collins was away that morning and so when Dr Debbie Allen saw my condition, she told me to immediately cease taking Abacavir as I had experienced a hypersensitivity reaction and to urgently contact Dr Mark Boyle (my HIV prescriber in Newcastle) without delay. I contacted Dr Boyle and he agreed with Debbie’s prompt advice and wanted me to also cease taking Kivexa. Two days later Abacavir and Kivexa were replaced by Truvada, which may have contributed to other problems a year later. This was the last of eight changes in my HIV antiretroviral medication over a nineteen-month period with my CD4 count then being 40.
The colonoscopy/endoscopy went ahead as scheduled on 30 May 2006 and those revealed my second AIDS defining opportunistic infection in eight years. This was severe candida oesophagitis involving the upper and middle oesophagus. My symptoms resolved relatively quickly after an immediate course of the anti-fungal drug Fluconazole and fortunately, there was no evidence whatsoever of either KS or MAC infections. Once again, my troublesome symptoms were blamed in part on my HIV antiretrovirals and very low CD4 count.
Unbeknown to me at the time, Dr Allen was so concerned about my declining health state, that she contacted a colleague at St. Vincent’s Hospital Immunology B and Ambulatory Care (IBAC) unit, who several years earlier had done a HIV Registrar placement at HSC to see if I could be reviewed and/or suitable for any HIV antiretroviral drug trials that were happening at St. Vincent’s at the time. Consequently, I had my first appointment with Dr Sara Pett on the 8 June 2006 when my CD4/VL counts was 22/451,000. Sara and I had an immediate rapport, and nothing was too much trouble for her. I came to Australia when I was three years old in 1958 and both of us being born in England might have had something to do with this. She was amazed when I walked into her office armed with my own complete HIV antiretroviral medication and results spreadsheet which covered my complete thirteen-year HIV history.
Sara successfully secured me one of the last places available in the two-year MK-0518 (Raltegravir)/placebo double blind trial in combination with boosted Darunavir, Ritonavir, Truvada and my old friend AZT which I had not taken since 1997. My results over the next six months were nothing short of amazing and according to Sara, I experienced a ‘phenomenal immune restoration’ because of my change in HIV antiretroviral therapy on the study. She felt sure that I must have been on the non-placebo Raltegravir because I had done so well on the study. If I had have been on the placebo Raltegravir, this would have not been expected with the amount of HIV virus resistance I had. Despite successive trending undetectable viral load counts, Sara was not optimistic that my CD4 counts would ever get as high as 500. Because I was locked into a two-year drug trial and doing remarkable well from the outset, I transferred my HIV care to Dr Sarah Pett and was extremely grateful for her care and ongoing support.
2007: Blaming HIV antiretrovirals, water works and bad bones
Sixteen months after starting the MK-0518 trial, Sarah sent me for a thoracic spine x-ray because at the time it reported that people taking Truvada were experiencing a decrease in their bone mineral density. At that stage I had been taking Truvada since May 2006 (when seeing Dr Boyle). I was very surprised when Sarah rang me in November 2007 with the bone density result, which revealed that I had a definite compression fracture at T7 and possibly at C6. I had not experienced any back pain or trauma. Sarah went on to tell me that I was borderline for having Osteoporosis (or in other words, Osteopenia). I was referred to Dr Yvonne Selecki who was a specialist at the Bone and Mineral Research for the Garvan Institute of Medical Research. Initially I treated with Actonel Combi and my ongoing management for Osteopenia was transferred to my local GP. For the next five years I was treated with Actonel Combi and Caltrate before my GP suggested I was eligible to treated with a once-yearly infusion of the drug Aclasta. I changed GPs five years later and continued with the infusions annually until my GP decided that I had been on this medication too long and needed to have a break. I did what I was asked to do, and my GP wouldn’t authorise a new script for Aclasta a year later until I had a long overdue Dexa Scan. A follow-up scan at St. Vincent’s in February 2022 revealed that my bone density had improved however, I was still classified as having Osteopenia. Unfortunately, I’m no longer eligible for yearly infusions and so am being solely managed by taking Caltrate alone. I must wait until age 70 before being eligible for other treatments that don’t cost the earth.
On top of this I was experiencing nocturia and was referred to a local Urologist, Dr Mark Louie-Johnsun who diagnosed me with Benign Prostatic Hyperplasia (BPH). All other tests for prostate cancer were normal. I was prescribed the drug Flomaxtra which helped my nocturia, but did not reduce the size of my enlarged prostate. At the time a surgical possibility was discussed, and I chose to remain on the medication for as long as I could. A couple of years later my medication was reduced however, surgery became necessary twelve years later in 2020.
There have only been four ‘blips’ on my V/L radar in the sixteen years since I first walked into Sara’s office. These only needed very minor adjustments to my HIV antiretroviral regimens by replacing AZT, Tenofovir and Truvada with 3TC and Etravirine.
I have remained on the same regimen (five medications/nine pills daily) for the past eight years. A far cry from my very early disastrous treatment journey. I feel envious of those of you that can tolerate monotherapy, I believe that for me, ‘it is what it is’.
2008: ‘On the buses’ – Run in for a sexual health check up
In mid-2008, HSC introduced a male specific after-hours sexual health clinic for men who could not get to the clinic during its regular operating hours. This was called the Gosford ‘Guys Clinic’ and was staffed by Michael Williamson (Registered Nurse) with administration support by me on Thursday evenings.
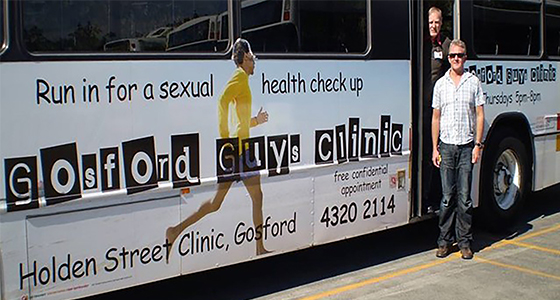
This clinic was very popular with men, especially those that commuted for work to either Sydney or Newcastle. Julie Asprey and Cindy O’Casey from our HIV/Sexual Health Promotion Team very successfully organised advertising with signage taking up the complete lengths of one side each of two Busways buses servicing routes around the Central Coast. The signs featured an Indigenous male running with the caption ‘Gosford Guy’s Clinic – Run in for a sexual health check up’.
Julie, Cindy and I worked collaboratively with the rest of the HARP Team two years later when I joined the PSN, and Julie was also a volunteer on the PSN Board for several years before that and beyond 2010.
2010: Time to jump ship, but not HIV/AIDS
Because my HIV treatment plateaued in 2010, and life generally was good, I was once again thinking of reducing my work hours which at the time had crept up to 88 hours a fortnight since the introduction of the Thursday evening Guy’s Clinic. Fortunately, with time-in-lieu (TIL) and monthly ADOs, this relieved some of my stress. Despite this, I suddenly found myself itching to do something new because I’d achieved everything I needed to do in my position at HSC. At age 55, I qualified for early retirement on 5 January 2010, but wanted to still work part-time if I could. This was not possible to do at HSC and when the PSN advertised for a new Manager in May 2010. I applied and began employment as the sole employee/manager in June 2010. Effectively I did semi-retire as the position was initially 25 hours/week over four days and the organisation’s Board approved my request to work three days/week doing longer days.
By the time I joined PSN, people living with HIV were living longer due to improvements in HIV antiretroviral medication and were less reliant on the organisation’s care and support services. Despite having an ongoing triannual funding agreement with NSW Health, often it was difficult to make ends meet. I worked hard with the Board and volunteers to revitalise programs and activities that formed part of that agreement while also improving community development and HIV health promotion in collaboration with the HARP Team. Fortunately, the Positive Speaker Service was not affected and continued to enjoy ongoing success and was very popular with Central Coast High Schools which I wanted to continue supporting.
One of my first tasks was to complete arrangements for PSN/HUGS (HIV understanding and group support) annual retreat in September that year at Mary McKillop Educational Centre in Kincumber. I first visited this wonderful facility in 2000 when I was the Positive Life PSB co-ordinator. I had been invited to do a talk to members who were at the time doing a series of workshops at the retreat. My talk was not about living with HIV, but instead it was about the PSB project. The group were very enthusiastic and excited to hear that people living with HIV in Sydney were travelling the state telling their personal HIV stories. I returned to the Mary McKillop venue in 2002 when I took a group of PSB positive speaker trainees there for a residential training weekend.

The next huge change was re-locating from PSN’s rented premises at Point Frederick, to accept an offer from the then Northern Sydney Central Coast Health Service (NSCCAHS) HARP Manager, Graham Stone to move into (and rent) office space, sharing the facilities with the HARP Sexual Health Promotion Team. This arrangement saved the PSN scarce funding which then could be put to other services for local people living with HIV. HUGS was fundamentally PSN’s core group of support and was still hugely popular, so activities were outsourced to keep that going. This was very successfully done and PSN enjoyed supporting the community more fully. I enjoyed sourcing funding from outside of the NSW Health funding agreement and doing fundraising events with the Board and volunteers. A sizeable grant from the Sydney Gay and Lesbian Business Association (SGLBA) towards the end of 2010, was my first big success and ensured financial security for PSN activities for quite some time.
Towards the end of 2010 I hosted a group of TAFE students who were doing their Certificate 4 in Mental Health and their teacher, Carol Huggett, at the newly acquired PSN office in Ward Street, Gosford. Students were doing Community Services and NGO agency familiarisation, and over the next five years I hosted many such visits. I somehow managed to find the time over the next four years to then go on to volunteer my time doing TAFE course validation as an ‘Industry expert’. Consequently, I was head-hunted to become a part-time casual teacher for TAFE NSW in 2015, after obtaining my TAE qualification. Carol joined the PSN Board in 2011 and remained as Secretary until the Board elected to close the organisation permanently in December 2015 after almost 25 years’ service for Central Coast people living with HIV (more in Oct ‘22 Talkabout). By the time this edition of Talkabout is published I will have clocked up another year as positive person (29 years).
In the next edition I will write about the period 2011–2016, back to the future, Sara’s return to UK, PSN Red Event, HAND, four-day cruise to nowhere, AIDS 2014 Melbourne, billboards and time capsule, adult education and myocardial infarction.
Paul R Maudlin OAM, JP
Published in Talkabout #204 August 2022






